Today, many women attend childbirth classes, physiotherapy or exercise groups for pregnant women. Do you want to know what therapeutic exercise for pregnant women really is? What does it consist of and when can it be done? Then keep reading this post and we will tell you.
The first thing we want to clarify is that we are always going to talk about therapeutic exercise (whether during pregnancy, postpartum or in any other area), since it is what we, as physiotherapists in Dwarka, carry out in our clinic. In a very brief way and without going into details, the difference is that our objective is to prevent and/or improve pathologies or injuries; that is, it always has an approach from the field of health, taking into account possible contraindications and adapting the exercise to posture, biomechanics, injury, ailment, etc. that each patient presents.
Returning to pregnancy, there are more and more studies that deny that pregnant women should avoid physical exercise because it could put the baby at risk. Well, today we know that this is not the case at all, and in fact, it is more than recommended that pregnant women maintain an active life, as long as there is no contraindication for it.
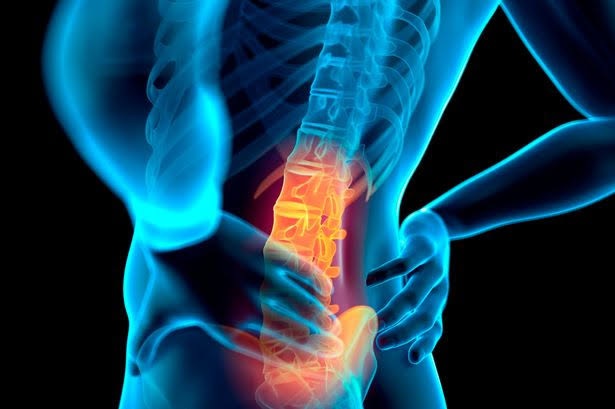
And that is precisely what therapeutic exercise for pregnant women is about. Its main objective is to keep the body in the best possible condition at a time when it is going through so many changes. In addition, it seeks to prepare the different tissues for the moment of delivery, and thus avoid possible complications or sequelae. Another very important point in these groups is postural correction and relaxation of the different joints and muscles, always with care, since laxity is increased at this stage.
And how is this achieved?
At Dr Sarwar Physiotherapy Center in Dwarka, we have brought together our knowledge of anatomy, different training methods and musculoskeletal techniques to develop a complete program of therapeutic exercise in pregnancy. Throughout the sessions, we will work on different aspects so that pregnancy and childbirth are carried out in the best possible way.
How do we do it?
- Initial assessment of each patient, to know what each member of the group needs.
- 1h classes, you can choose between 1 or 2 sessions/week.
- Small groups (maximum 5 people).
- Individualized exercises are controlled at all times by a physiotherapist.
Class structure:
- Heating.
- Strength exercises give special importance to the transverse and pelvic floor.
- Flexibility and joint mobility exercises are important to favour the baby’s positioning for childbirth and prepare our body for that moment.
- Postural exercises, including therapeutic pilates exercises.
- Stretching and relaxation techniques.
When can I start?
Because it is a preventive program, it should be started as soon as possible, after the first 3 months, which are the highest risk for the embryo. In general, this type of exercise is usually started between the 14th and 16th week of gestation, at which time the fetus is already developed (although it continues to grow) and in which there is still time to prevent neck pain. back and other disorders.
What will it help me with?
- improve posture
- Prevent and/or relieve pain associated with pregnancy.
- Make the pelvic joints more flexible to favour their opening in childbirth, and tone and elasticize the pelvic floor.
- Provide relaxation and breathing techniques useful during pregnancy and childbirth.
- Share time with women in the same state as you and share concerns and experiences.
Am I a candidate to join a group?
This program, as its name suggests, is intended for any woman who is expecting a baby. As with any training method, there are a number of contraindications. The most important thing is that you pay attention to your gynaecologist if she gives you rest for any reason.
If you have doubts, you can consult a physiotherapist in Dwarka without any problem and we will tell you if it is contraindicated in your case or not.
Now there is no excuse not to keep your pregnant body active and, at the same time, enjoy the process of preparing for childbirth. If you do, you will notice the difference, we assure you.